Trigeminal Neuralgia
Conditions, Symptoms, Diagnosis, Treatment and Best Options and Best Surgeon for Trigeminal Neuralgia Treatment in Pune
Imagine experiencing the worst pain imaginable – a sudden, excruciating electric shock, like a thousand knives stabbing your face, triggered by a light touch, a cool breeze, or even talking or chewing. This is the reality for individuals suffering from Trigeminal Neuralgia (TN), often referred to as the “Suicide Disease” due to its unbearable agony and profound impact on quality of life. This chronic pain condition affects the trigeminal nerve, one of the most important nerves in the face, responsible for transmitting sensations from the face to the brain.
For those grappling with this debilitating condition, hope and relief are paramount. In Pune, India, Dr. Jaydev Panchwagh, a world-renowned neurosurgeon, has emerged as a leading expert in the treatment of Trigeminal Neuralgia, with extensive experience in Microvascular Decompression (MVD) surgery, offering a chance at a permanent cure for countless patients both nationally and internationally.
What is Trigeminal Neuralgia?
Trigeminal Neuralgia is a chronic pain condition affecting the trigeminal nerve, also known as the 5th cranial nerve. There are two trigeminal nerves, one on each side of the face, each with three main branches that supply sensation to different parts of the face, gums, and teeth:
- Ophthalmic (V1): Controls sensation in the forehead, eye, and upper part of the nose.
- Maxillary (V2): Controls sensation in the cheek, upper jaw, upper teeth, and upper lip.
- Mandibular (V3): Controls sensation in the lower jaw, lower teeth, lower lip, and part of the ear.
“Neuralgia” simply means nerve pain. Therefore, Trigeminal Neuralgia is pain in the region supplied by the trigeminal nerve, typically on one side of the face. This pain is not a dull ache, but rather a sudden, severe, and episodic pain that can feel like an electric shock, stabbing, piercing, or a burning sensation.
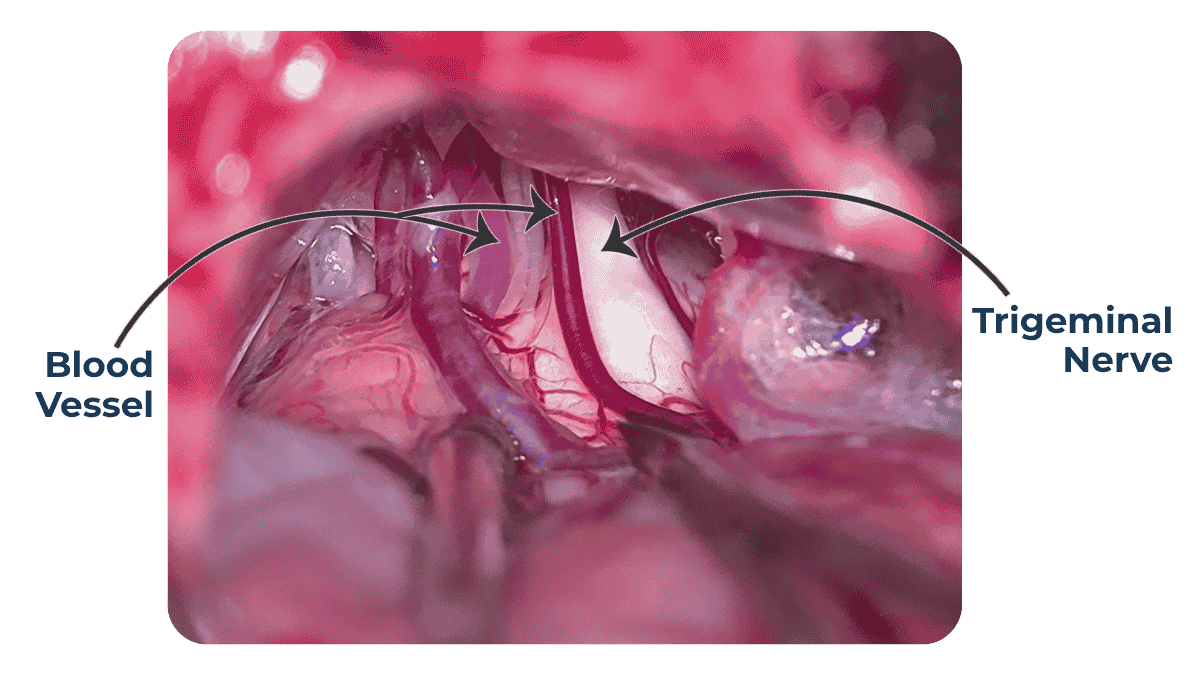
The most common cause, as thoroughly explained by Dr. Jaydev Panchwagh, is compression of the trigeminal nerve by a nearby blood vessel (usually an artery) where the nerve exits the brainstem. Over time, the continuous pulsations of this vessel against the nerve can damage its protective insulation (myelin sheath), causing the nerve impulses to misfire, leading to the agonizing pain. Less commonly, it can be caused by conditions like Multiple Sclerosis or, very rarely, by a tumor displacing a blood vessel against the nerve.
- Symptoms
- Causes and Risk
- Diagnosis
- Treatment
Diagnosing Trigeminal Neuralgia is primarily a clinical diagnosis, meaning it relies heavily on the patient’s detailed description of their symptoms and medical history. Dr. Jaydev Panchwagh emphasizes the importance of carefully listening to the patient’s unique pain story, as the typical characteristics of the pain are often sufficient for diagnosis.
The diagnostic process typically includes:
- Detailed Medical History and Symptom Review: The neurosurgeon will ask extensive questions about the nature, location, severity, frequency, and triggers of your pain. The patient’s facial contortions and defensive posturing during conversations can also provide immediate clues.
- Neurological Examination: This involves assessing reflexes, sensation, and motor function of the face to identify any abnormalities or rule out other conditions.
- Imaging Tests (MRI): While Trigeminal Neuralgia is a clinical diagnosis, an MRI of the brain is crucial. Dr. Panchwagh often uses a special “Trigeminal Neuralgia protocol MRI” with 3D reconstruction. This specialized MRI helps:
- Visualize the nerve and surrounding vessels: To identify if a blood vessel is compressing the trigeminal nerve, which is the most common cause.
- Rule out other causes: To ensure the pain isn’t due to a Tumor, multiple sclerosis lesion, or other structural abnormalities affecting the nerve.
Aid surgical planning: If Microvascular Decompression (MVD) is considered, the MRI provides vital anatomical details for the surgeon.
Understanding what causes Trigeminal Neuralgia (TN) is crucial in finding the right treatment path. According to Dr. Jaydev Panchwagh—an internationally recognized expert in treating this condition—the primary cause of Trigeminal Neuralgia is compression of the trigeminal nerve by a nearby blood vessel, most commonly an artery, near the brainstem. This compression damages the myelin sheath, the protective covering of the nerve, leading to abnormal nerve signaling and the agonizing, electric-shock-like facial pain that defines this disorder.
Most Common Cause: Vascular Compression
Arterial Loop Compression: In the majority of cases, a blood vessel continuously pulsates against the trigeminal nerve where it exits the brainstem. Over time, this repetitive pressure causes the protective myelin layer to wear away, resulting in misfiring of nerve signals and excruciating pain episodes.
Venous Compression: Less commonly, a vein may be involved in the compression, either alone or in combination with an artery.
This compression-based cause is why Microvascular Decompression (MVD) is the most effective and potentially curative treatment, as it addresses the root mechanical issue.
Other (Less Common) Causes
Multiple Sclerosis (MS): In some patients, especially those under 50, Trigeminal Neuralgia may be a symptom of MS, a neurological condition that causes demyelination within the central nervous system, including the trigeminal nerve root.
Tumors: Very rarely, a brain tumor may press against the trigeminal nerve or shift nearby blood vessels, causing secondary compression.
Cysts or Structural Abnormalities: Developmental or acquired abnormalities near the nerve origin can also lead to irritation or compression.
Post-Traumatic Injury: Facial trauma or prior surgeries may damage the nerve or surrounding structures, potentially leading to neuralgia symptoms.
Risk Factors
While Trigeminal Neuralgia can affect anyone, several risk factors may increase the likelihood of developing the condition:
Age: Most commonly affects individuals over 50 years of age, although it can occur earlier, especially in MS-related cases.
Gender: Women are more frequently affected than men.
Family History: A genetic predisposition has been suggested in some familial cases, although it’s rare.
Neurological Disorders: Conditions like Multiple Sclerosis increase the risk of TN.
Previous Facial Trauma or Surgery: Past injuries or procedures involving the skull base or facial structures may contribute to trigeminal nerve irritation.
Diagnosing Trigeminal Neuralgia is primarily a clinical diagnosis, meaning it relies heavily on the patient’s detailed description of their symptoms and medical history. Dr. Jaydev Panchwagh emphasizes the importance of carefully listening to the patient’s unique pain story, as the typical characteristics of the pain are often sufficient for diagnosis.
The diagnostic process typically includes:
- Detailed Medical History and Symptom Review: The neurosurgeon will ask extensive questions about the nature, location, severity, frequency, and triggers of your pain. The patient’s facial contortions and defensive posturing during conversations can also provide immediate clues.
- Neurological Examination: This involves assessing reflexes, sensation, and motor function of the face to identify any abnormalities or rule out other conditions.
- Imaging Tests (MRI): While Trigeminal Neuralgia is a clinical diagnosis, an MRI of the brain is crucial. Dr. Panchwagh often uses a special “Trigeminal Neuralgia protocol MRI” with 3D reconstruction. This specialized MRI helps:
- Visualize the nerve and surrounding vessels: To identify if a blood vessel is compressing the trigeminal nerve, which is the most common cause.
- Rule out other causes: To ensure the pain isn’t due to a tumor, multiple sclerosis lesion, or other structural abnormalities affecting the nerve.
Aid surgical planning: If Microvascular Decompression (MVD) is considered, the MRI provides vital anatomical details for the surgeon.
The goal of Trigeminal Neuralgia treatment is to alleviate the excruciating pain and improve the patient’s quality of life. Treatment options range from medication to advanced surgical procedures, with Dr. Jaydev Panchwagh emphasizing a tailored approach for each patient.
- Medication:
- First-Line Treatment: Anticonvulsant medications, such as Carbamazepine (Tegretol) and Oxcarbazepine, are typically the first line of treatment. They work by calming abnormal nerve activity.
- Adjunctive Medications: Other drugs like Gabapentin or Baclofen may be used in combination to enhance pain relief or manage side effects.
- Limitations: While effective initially, medications often lose their efficacy over time, requiring higher doses. These higher doses can lead to significant side effects like dizziness, fatigue, nausea, confusion, and even violent dreams, impacting daily function. As Dr. Panchwagh states on trigeminalneuralgiatreatment.org, “no medicine can act on just one nerve. It therefore acts on the entire nervous system, numbing it. This is the primary reason for the major side-effects of medication.”
- Surgical Options (Best Options for Long-Term Relief/Cure):
- Microvascular Decompression (MVD) Surgery:
- The Gold Standard and Potentially Curative: MVD is widely considered the most effective long-term treatment and the only potentially curative option for Trigeminal Neuralgia. Dr. Jaydev Panchwagh is an international authority in MVD surgery, having performed over 2000 MVD procedures, one of the largest series in India, making his center a “Centre of Excellence” for TN treatment.
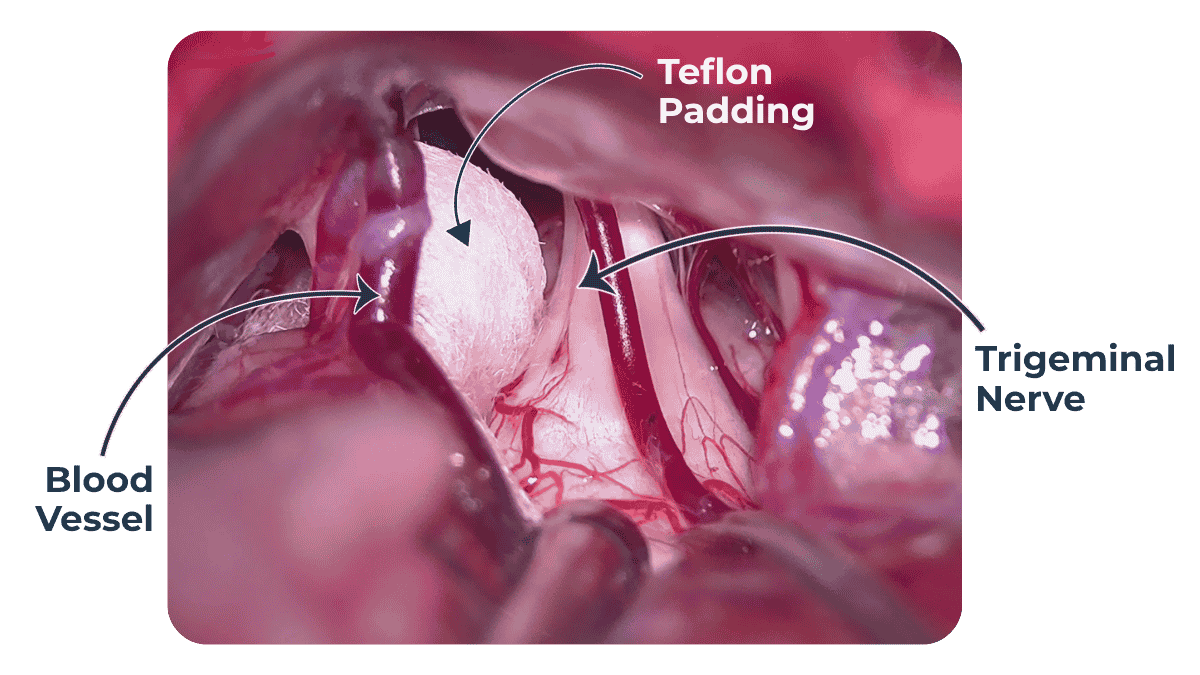
- How it Works: Performed under a neurosurgical microscope, a small opening is made behind the ear. The neurosurgeon then carefully identifies the blood vessel (usually an artery) that is compressing the trigeminal nerve. This vessel is gently moved away from the nerve, and a small, permanent Teflon sponge is inserted between them to prevent future contact and compression.
- Benefits: MVD aims to address the root cause of the pain. It offers immediate or rapid pain relief in a very high percentage of patients (often over 95%), with the potential for long-term or permanent cure. Crucially, it preserves normal nerve function and avoids nerve destruction, meaning no permanent facial numbness in most cases. Dr. Panchwagh strongly advocates for MVD early in the disease course, before irreversible nerve damage from prolonged medication use or destructive procedures.
- Gamma Knife Radiosurgery:
- Non-Invasive Radiation: This technique uses highly focused beams of radiation to damage the trigeminal nerve where it enters the brainstem, thereby disrupting pain signals.
- Considerations: It is non-invasive, but relief can take weeks to months, and the effect is generally temporary (pain may recur after a few years). It causes some degree of nerve destruction, which can lead to facial numbness.
- Radiofrequency Lesioning (RFL):
- Minimally Invasive Destruction: A thin needle is inserted through the cheek to the trigeminal ganglion at the skull base. Radiofrequency energy is used to selectively burn and destroy the pain-carrying nerve fibers.
- Microvascular Decompression (MVD) Surgery:
Considerations: This is also a destructive procedure. While offering quick relief, it often leads to facial numbness and the pain tends to recur, sometimes within months or a few years. Dr. Panchwagh notes that performing RFL primarily can sometimes reduce the success rate of a subsequent MVD.
Watch this Video to Know More about Trigeminal Neuralgia
Why Choose Dr. Jaydev Panchwagh for Trigeminal Neuralgia Treatment?
When faced with the unbearable pain of Trigeminal Neuralgia, choosing the right neurosurgeon is of utmost importance. Dr. Jaydev Panchwagh’s reputation as a world leader in MVD surgery makes him a preferred choice for patients seeking lasting relief:
- Unparalleled Experience in MVD: With over 2900 MVD surgeries performed for both Trigeminal Neuralgia and Hemifacial Spasm, Dr. Panchwagh possesses one of the largest single-surgeon experiences in India, establishing his center as a “Centre of Excellence.” This volume translates to exceptional skill and refined that provides best results for his patients that provides best results for his patients.
- Focus on Long-term Cure: Dr. Panchwagh passionately advocates for MVD as the best chance for a Long-term cure, unlike temporary relief offered by nerve-numbing medications or destructive procedures. He emphasizes the importance of early MVD intervention to prevent brain changes due to exposure to chronic pain and effect of medication.
- Minimizing Side Effects: His MVD approach aims to preserve normal nerve function, thereby avoiding many problems. often associated with destructive procedures and allowing patients to stop “brain-numbing” medications with their debilitating side effects.
- International Recognition and Referrals:Patients from more than 22 Indian states and around 15 countries across the globe have travelled to Pune to receive his specialized treatment for Trigeminal Neuralgia—an enduring testament to his international reputation and expertise.
- Comprehensive Patient Support: Through the Synapse Brain and Spine Foundation and his dedicated team, Dr. Panchwagh ensures patients receive not just surgical excellence but also thorough counseling, pre- and post-operative care, and guidance for medicine tapering.
Educator and Advocate: Dr. Panchwagh is a recognized teacher and actively educates patients and the public about Trigeminal Neuralgia through seminars, publications, and online platforms.
Frequently Asked Questions (FAQs) about Trigeminal Neuralgia
While it’s a chronic condition, treatments like Microvascular Decompression (MVD) surgery offer the potential for a long-term or permanent cure, allowing many patients to live pain-free.
Trigeminal Neuralgia is often mistaken for dental pain, leading to unnecessary tooth extractions. While dental issues can cause facial pain, the sharp, electric-shock-like nature and specific triggers of TN are distinct. A proper diagnosis by a neurosurgeon is crucial.
Most patients are discharged from the hospital within 2-4 days after MVD surgery. Full recovery and return to normal activities typically take a few weeks. Dr. Panchwagh’s team provides specific post-operative guidance.
After a successful MVD surgery, which is generally to be expected, Dr. Jaydev Panchwagh and his team will guide you through a specific protocol to gradually taper off your pain medications over several weeks, aiming for you to become medicine-free.
Do not let the unbearable pain of Trigeminal Neuralgia define your life. With the advanced expertise and compassionate care offered by Dr. Jaydev Panchwagh, a path to lasting relief and recovery is within reach.

A distinguished Brain and Spine Surgeon, shaping neurosurgical care in Pune, Maharashtra, India for over two decades.
Quick Link

Quick Contacts
- Phone : (+91) 9011333841 , (+91) 7720948948
- brainspine66@gmail.com
- 102, Bhagyatara Society, 1st floor, Mehendale Garage road, Erandwane, Pune
Map
- Copyright @2025 | Dr. Jaydev Panchwagh | Praavi Medicare
